Unlocking Peak Performance: The Ultimate Guide to TRT Protocols
For Private Companies or Public Healthcare
Foreword
As a doctor, I have been asked to write a pathway for TRT prescribing
I am not currently in the ‘TRT’ space i.e. I am not prescribing TRT to people
I have not ruled out entering the field, whether through launching my own startup or by joining another one
Much of this will relate to the ideal pathway within a private setting, though the NHS could/would mimic the same design.
Quick note on the ‘normal’ range
There are actually different ranges considered as ‘normal.’ The attributed normal range changes depending on the lab taking the test, and the country that you are in…
Usual NHS range:
Male: 6 - 27 nmol/L
Female: <2.7 nmol/L
Average US range:
Male: 10 to 35 nmol/L
Female: 0.5 to 2.4 nmol/L
In males, after the age of 40 testosterone levels generally decline by 1 to 2% on average each year. 90% of men with low testosterone remain undiagnosed.
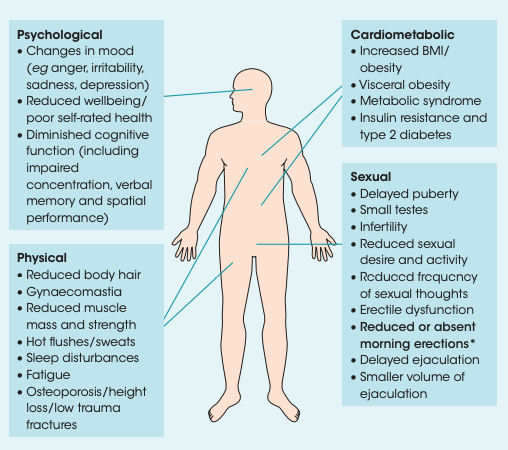
The symptoms of testosterone deficiency are as follows:
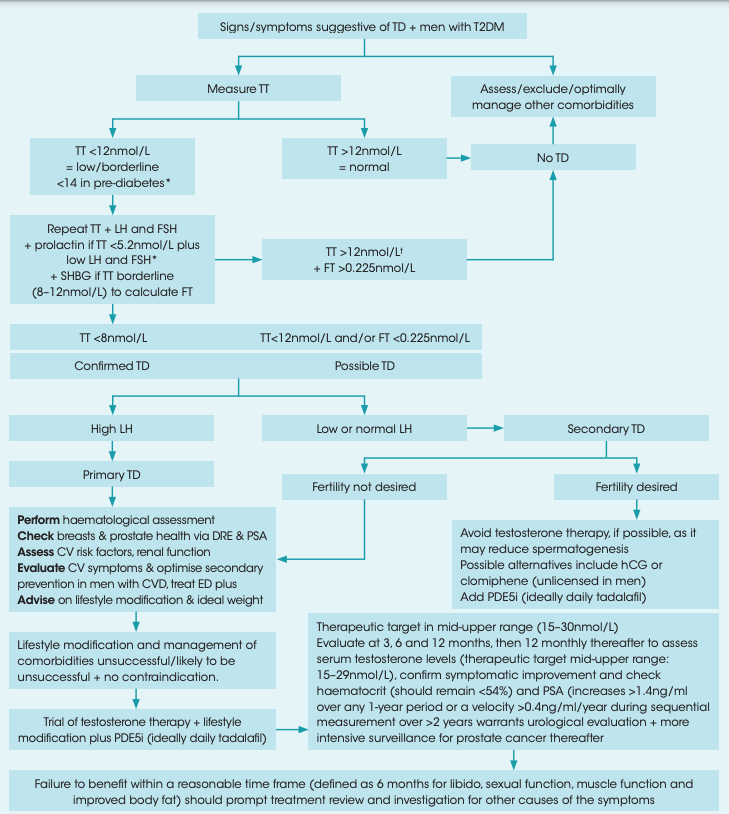
Pathway for Delivering TRT:
Patient Onboarding and Initial Assessment
Consultations: Offer both digital and in-person consultations with registered medical professionals.
TRT assessment portal: Create a digital portal where patients provide detailed information on symptoms (fatigue, low libido, mood changes), medical history, and lifestyle.
Understanding Intent: Assess why the patient wants TRT. Are they seeking to correct hormone imbalances from past steroid abuse, or are they symptomatic of hypogonadism?
Mental Health Screening: Conduct a thorough mental health evaluation, focusing on potential body dysmorphia, addiction behaviours, or psychological dependence on anabolic steroids.
Physical examination considerations: height, weight, BMI, waist circumference, degree of body hair, abnormalities of penis/testis/scrotum, DRE
Initial Diagnostic Testing:
Comprehensive blood tests are mandatory before any diagnosis:
Morning total testosterone levels (measured on at least two occasions, preferably 4 weeks apart).
Additional tests for LH, FSH (pituitary function), SHBG, free testosterone, prolactin, thyroid function, liver function, lipid profile, and haematocrit.
LH, FSH to evaluate pituitary function and distinguish between primary and secondary hypogonadism
SHBG to calculate Free Testosterone
PSA for men over 40 or those with a family history of prostate cancer.
Total testosterone levels are not as useful as free testosterone. The latter is the one you should want to optimise.
Note: Physiological testosterone follows a diurnal rhythm. Therefore measurements are most useful if tests are taken around the same time on each occasion e.g. 07:00 - 11:00am
Diagnostic packages can be sent to the patient’s home for remote blood collection or arranged at a partner lab for convenience.
To have a low ‘entry-fee’ for consumers, it might be beneficial to have two blood tests prior to assessment. The first would be a Total testosterone test, to exclude those with a normal level. If Total testosterone is low or borderline, then the whole panel would be taken.
However, for those who want the whole panel from the start (note that I did mention that free testosterone is much more useful), they should be allowed to exclude the initial test and go straight to the full-panel.
Personalised Treatment Plan
Consultation with a Specialist:
Following diagnosis, patients meet with a TRT-specialised clinician (in-person or remotely) to discuss results and treatment options.
Emphasise shared decision-making, with thorough discussions around:
Benefits: improved mood, energy, muscle mass, and sexual function.
Risks: potential for polycythaemia, cardiovascular events, prostate issues.
Exclusion criteria: active cancer, untreated sleep apnoea, or severe psychiatric issues must be identified and managed.
Family history of prostate or breast cancer must be factored into decisions.
Fertility aspirations: Also consider the desire to have children
Tailored TRT Regimen:
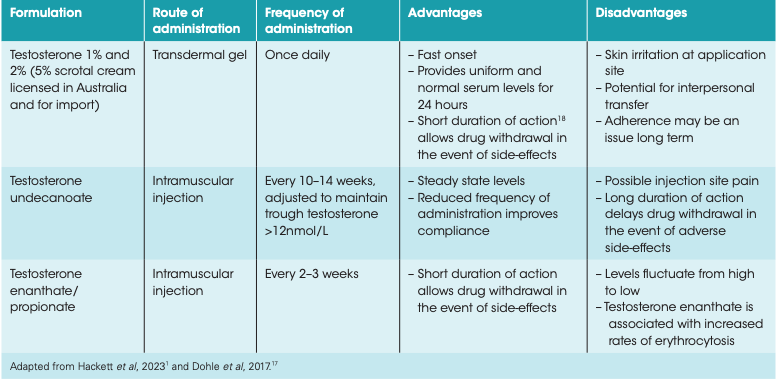
The prescription depends on patient preference, lifestyle, and medical history. See below
Ensure the patient is aware that this is a long journey and a gradual process. A dose will be given, testosterone will be measured again, then the dose will be titrated upwards…
Initial Treatment and Monitoring
Initial Dosing and Adjustment:
Start TRT with the lowest effective dose and titrate based on clinical response and blood levels.
Patients should be scheduled for regular blood tests after starting treatment to assess:
Serum testosterone levels.
Haematocrit, lipid profile, liver function tests, and PSA (as applicable).
Blood tests at: 6 weeks, 3 months, 6 months, 12 months.
Patient Education:
Patients are provided with comprehensive education materials (digital and paper) on how to administer their treatment, monitor side effects, and adjust their lifestyle to improve outcomes.
Offer 24/7 digital access for queries or concerns, improving patient satisfaction and adherence.
Long-Term Care and Optimisation
Regular Monitoring Protocol:
Once stabilised, patients should have biannual consultations and regular blood tests every 6-12 months.
A focus on preventing complications:
Monitor haematocrit levels to avoid polycythaemia.
Regular cardiovascular assessments, particularly in older patients.
Mental health assessments to monitor for mood swings, anxiety, or depression (linked to hormonal changes).
Digital Monitoring and Support:
Utilise the digital platform to provide personalised feedback based on blood test results, symptoms, and patient-reported outcomes.
Automated reminders for medication administration, follow-up appointments, and blood tests.
Psychological and Mental Health Support
Access to Counselling and CBT:
Offer integrated or signpost to mental health support for patients with a history of anabolic steroid abuse or psychological disorders (e.g., body dysmorphia).
Provide options for cognitive behavioural therapy (CBT) or addiction counselling where required.
Wellness Packages:
Complement TRT with additional wellness services, including nutritional counselling, personal training plans, and lifestyle coaching to promote overall health improvement beyond hormone replacement.
Could upsell, or provide free to increase user satisfaction. Dependent on how thorough these services are
Scalable Model for Growth
Subscription-Based Service:
Implement a subscription model where patients pay a flat monthly fee that includes all consultations, blood tests, medications, and support services.
Offer tiered services (e.g., basic TRT vs. premium packages with enhanced wellness offerings).
Clinic Expansion:
Begin with flagship clinics in major cities, focusing on regions with higher demand for private healthcare.
Expand via partnerships with independent labs, gyms, or health centres to offer remote blood testing and consultations across the country.
Partnerships and Brand Building:
Collaborate with influencers, sports organisations, or fitness communities to build brand credibility and trust.
Maintain strong clinical governance and ethical standards to distinguish the brand as a reputable, safe provider in an industry sometimes associated with unregulated treatments.
Prescribing Protocol for TRT:
Eligibility and Diagnostic Criteria
Age: Typically men over the age of 30 with documented symptoms of hypogonadism or significant hormone imbalances (e.g. caused by past anabolic steroid abuse)
Lab Confirmation: Morning total testosterone levels < 12 nmol/L on at least two occasions, preferably 4 weeks apart
Symptomatology: Presence of key symptoms such as low libido, fatigue, depression, or loss of muscle mass.
Exclusion Criteria: Active or suspected prostate cancer, severe cardiovascular disease, polycythaemia, untreated sleep apnoea, or untreated psychiatric conditions. Consider family history of above.
TRT Options
Intramuscular Injection:
Testosterone enanthate or cypionate (100-200 mg/2 weeks).
Testosterone undecanoate (Nebido®) 1000 mg/10-14 weeks.
Transdermal Gel or Patches:
Daily application of 50–100 mg gel (Androgel® or Testogel®) or patch for non-invasive treatment.
The perfect TRT protocol should as closely replicate the patient’s natural physiological levels at their peak. To achieve this, usually one starts at a low dose and aims to titrate up over time.
If you are aromatising too much testosterone, then your dosage might be too high. I’m not entirely sure that aromatase inhibitors are within our medical guidelines, so I will not be delving into them here. Same as for HCG (an LH analogue). Discussion will remain on Testosterone.
Follow-Up and Monitoring
a. Blood tests every 3-6 months during the first year, then annually, assessing testosterone levels, haematocrit, liver function, and lipid profile.
b. Review consultations every 3-6 months to adjust dosage or switch to alternative formulations based on clinical response.
c. Psychiatric and psychological evaluation on a routine basis, especially for patients with prior anabolic steroid use.
BSSM Pathway
Considerations regarding TRT dosing outside standard medical guidelines
In clinical practice, TRT is typically prescribed based on standardised dosing regimens aimed at achieving stable serum testosterone levels within the normal physiological range. However, there are nuanced approaches to TRT dosing, particularly with regard to reducing side effects such as aromatisation (conversion of testosterone to oestrogen) and 5-alpha reductase effects (conversion of testosterone to dihydrotestosterone or DHT).
These are not explicitly found in medical guidelines, so while I’m happy to share some thoughts for informational purposes, I’m not putting my medical licence on the line for them!
Micro-dosing
The concept of "micro-dosing" refers to administering smaller doses of testosterone more frequently, rather than using larger doses at longer intervals. This strategy arguably has several potential advantages over guideline dosages, particularly in mitigating unwanted side effects associated with TRT:
1. Reduction of Aromatisation (Testosterone to Oestrogen Conversion)
Testosterone can be converted to oestrogen via the enzyme aromatase, particularly in adipose tissue. This conversion can lead to increased levels of oestradiol, potentially causing side effects such as gynaecomastia (breast tissue development in men), water retention, and mood swings.
Larger doses of testosterone given at longer intervals can cause peaks in serum testosterone levels, leading to more aromatisation during the peak periods.
By administering smaller, more frequent doses, the peaks and troughs of testosterone levels are minimised. This reduces the chances of high serum testosterone concentrations that can trigger increased aromatisation.
2. Reduction of 5-Alpha Reductase Effects (Testosterone to DHT Conversion)
Testosterone is also converted to dihydrotestosterone (DHT) via the enzyme 5-alpha reductase, particularly in the skin, liver, and prostate (locally).
Elevated levels of DHT can contribute to androgenic side effects, such as acne, male pattern baldness, and prostate enlargement.
Similar to aromatisation, when large doses of testosterone are given intermittently, the higher peak levels may lead to increased conversion to DHT.
Smaller, more frequent doses reduce the testosterone surges that drive DHT production. This results in lower average DHT levels, potentially decreasing androgenic side effects like acne and hair loss.
3. Improved Symptom Control and Patient Experience
Anecdotally, TRT patients report that testosterone fluctuation causes symptoms including fatigue, irritability, and mood swings
Micro-dosing ensures a more consistent release of testosterone, which can lead to more stable mood and energy levels, providing better overall symptom control.
However, increased dosing frequency requires more injections or applications, which may be less convenient for patients, resulting in adherence issues.
Again, I am not in the TRT space (yet?). I am not risking my medical licence to ‘recommend’ the above, as opposed to standard guidelines. It is for informational purposes only.
Does testosterone actually increase the risk of prostate cancer?
Short answer: it’s debatable.
Under NHS guidelines, the answer is a yes. Higher free testosterone will increase the risk of prostate cancer. However, there is a possibility of detection bias in this.
Some studies show that using TRT to maintain serum T levels within the ‘normal range’ actually decreases the risk of prostate cancer.
Two papers have been added to the references, for one to look into this further.
Key Considerations for a Private Company Entering the TRT Space:
Regulatory Compliance:
Ensure compliance with the Care Quality Commission (CQC) in England or equivalent regulatory bodies in the operating regions.
Adhere to General Medical Council (GMC) prescribing guidelines and the British Society for Sexual Medicine (BSSM) standards.
Establish proper licensing for handling and prescribing controlled substances like testosterone.
Patient-Centric Model:
Offer a seamless digital and physical infrastructure for patient interaction, from initial consultation to follow-up care, using telemedicine and in-person clinics.
Create a subscription-based service with transparent pricing, including diagnostic tests, treatment plans, and regular follow-ups.
Technology Integration:
Develop or utilise an existing digital health platform to streamline patient onboarding, assessment, and follow-up.
App-based reminders (or email / texts) for follow-up blood tests
References
The Journal of Clinical Endocrinology & Metabolism, Volume 92, Issue 11, 1 November 2007, Pages 4241–4247
https://bssm.org.uk/
Watts EL, Appleby PN, Perez-Cornago A, Bueno-de-Mesquita HB, Chan JM, Chen C, Cohn BA, Cook MB, Flicker L, Freedman ND, Giles GG, Giovannucci E, Gislefoss RE, Hankey GJ, Kaaks R, Knekt P, Kolonel LN, Kubo T, Le Marchand L, Luben RN, Luostarinen T, Männistö S, Metter EJ, Mikami K, Milne RL, Ozasa K, Platz EA, Quirós JR, Rissanen H, Sawada N, Stampfer M, Stanczyk FZ, Stattin P, Tamakoshi A, Tangen CM, Thompson IM, Tsilidis KK, Tsugane S, Ursin G, Vatten L, Weiss NS, Yeap BB, Allen NE, Key TJ, Travis RC. Low Free Testosterone and Prostate Cancer Risk: A Collaborative Analysis of 20 Prospective Studies. Eur Urol. 2018 Nov;74(5):585-594. doi: 10.1016/j.eururo.2018.07.024. Epub 2018 Aug 1. PMID: 30077399; PMCID: PMC6195673.
Zhang X, Zhong Y, Saad F, Haider KS, Haider A, Clendenin AG, Xu X. Testosterone therapy may reduce prostate cancer risk due to testosterone deficiency at a young age via stabilizing serum testosterone levels. Aging Male. 2020 Jun;23(2):112-118. doi: 10.1080/13685538.2019.1578739. Epub 2019 Mar 12. PMID: 30857458.
Closing Remarks
I AM a doctor, but this is not to be taken as clinical advice. Go to your doctor / a TRT-specialist doctor. This is for informational purposes only
If anybody wants to discuss TRT with me, for academic or business purposes, please get in touch via LinkedIn
Links
LinkedIn: https://www.linkedin.com/in/dr-jamil-shah-foridi/
Medium:https://drjams.medium.com/
Substack: https://drjams.substack.com/
Youtube (coming soon): https://www.youtube.com/channel/UCxHnvpvKuPbB1380X0h8ybA



I have now written a more extensive piece on TRT, including the size of the market, key players and also areas for innovation. Found here: https://drjams.substack.com/p/the-trt-playbook